Research has demonstrated certain correlations between COVID-19 severity and an array of comorbidities, and studies are now exploring the role of metabolomics and the microbiome in determining COVID-19 hospitalization.1 Previous research noted a connection between severity and specific cytokines, such as interleukin (IL)-6.2–4 Thus exploration of predictive biomarkers relating to COVID-19 severity could offer an opportunity to flag those prone to adverse outcomes.
Metabolomics and Multiomics Analysis for Predicting COVID-19 Severity
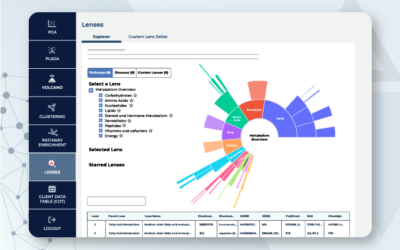
A retrospective cohort study comprised of 455 COVID-19 patients analyzed various predictive biomarkers for COVID-19 severity. For instance, the deep profiling included metabolites, lipids, circulatory cytokines, and other proteins.1 In particular, the study explored 1018 metabolites, 902 lipids, and 1463 cytokines and circulatory proteins to assess their connection to clinical and severe cases.1 Metabolon conducted the lipidomics for the study. Further, researchers leveraged proximity extension assays and tandem mass spectrometry for measurements of the biomarkers.1
In addition, the study included multiomics dataset analysis and machine learning algorithms for biomarker discovery. A select few previous studies combined machine learning with multiomics for COVID-19 severity research, but they were limited by smaller sample sizes than the current one.5,6
Machine-learning-based Prediction Model Identifies New Biomarkers
The research concluded that a machine-learning-based prediction model could accurately anticipate both clinical and severe COVID-19 outcomes with improved accuracy, as compared to traditional cytokine methods. Specifically, the study’s model noted a correlation with 102 predictive biomarkers for clinical and severe COVID-19 that included metabolites, lipids, and novel cytokines as well as additional proteins.1 In particular, these biomarkers included differing amounts of 2-hydroxydecanoate, C-type lectin domain family 6 member A (CLEC6A), and ether phosphatidylethanolamine (P-18:1/18:1).1
Further, the study’s metabolomic data showed that 12 of the 102 predictive biomarkers of COVID severity that changed were lipid-related. Additional nonlipid metabolomic markers identified by the research were heme and polyamines, which showed increases with disease severity. As well, the study combined proteomic cytokine storm markers with metabolomic markers, demonstrating the benefits of a complementary multiomic approach to biomarker discovery.
Additional research should explore validation of the findings that includes an independent control group cohort, but this study provides essential data supporting preliminary efficacy of the model and the key role of particular biomarkers in COVID-19 severity.
Study Implications for Multiomics Research
The findings suggest a benefit from exploring COVID-19 patients’ multiomic molecular signature from plasma prior to hospital admission.1 Doing so holds the potential to predict if the patient will suffer a more severe course of disease or not. Further, the study supports the idea that machine-learning approaches could potentially garner additional insights for clinical use by applying them to complex profiling data in additional disease areas.1
Compared to previous studies, this one was particularly well-powered with 455 cases and 182 controls. The study reported the important role of the microbiome and metabolites, as noted from the researchers’ identification of novel microbially-derived metabolite, imidazole propionate, which predisposes patients to poor COVID outcomes when levels are increased. In addition, the study has important implications regarding plasmalogens, which appear protective in this study. In summary, a multiomics analysis has the potential to drive additional research insights for COVID-19 and other diseases.
Ready to see what new insights metabolomics can help your research reveal?
Contact us today to discuss your project or study.
References
1. Byeon, S.K., Madugundu, A.K., Grapati, K., Ramarajan, M.G., Saraswat, M., Kumar-M, P., et al. Development of a multiomics model for identification of predictive biomarkers for COVID-19 severity; a retrospective cohort study. The lancet. 2022; 4(9), E632-E645. DOI:https://doi.org/10.1016/S2589-7500(22)00112-1
2. Rosas IO, Bräu N, Waters M, et al. Tocilizumab in hospitalized patients with severe COVID-19 pneumonia. N Engl J Med. 2021; 384: 1503–16.
3. Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021; 384: 693–704.
4. Group RC. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomized, controlled, open-label, platform trial. Lancet. 2021; 397: 1637–45.
5. Su Y, Chen D, Yuan D, et al. Multi-omics resolves a sharp disease-state shift between mild and moderate COVID-19. Cell. 2020; 183: 1479–95.
6. Overmyer KA, Shishkova E, Miller IJ, et al. Large-scale multi-omic analysis of COVID-19 severity. Cell Syst. 2021; 12: 23–40.