Case Study
Ketogenic Efficacy Through Microbiome Metabolism
Potential treatment for epilepsy without using probiotics is revealed through metabolomics following ketogenic diet treatment.
Metabolon identified hundreds of metabolites, with a large portion of those with significantly altered levels belonging to a class of metabolites called gamma-glutamylated amino acids (GG-AAs). The GG-AAs were found to be reduced in the seizure-protected mice, illuminating that the GG-AAs level was significantly correlated to the number of seizures in mice.
Metabolon identified hundreds of metabolites, with a large portion of those with significantly altered levels belonging to a class of metabolites called gamma-glutamylated amino acids (GG-AAs). The GG-AAs were found to be reduced in the seizure-protected mice, illuminating that the GG-AAs level was significantly correlated to the number of seizures in mice.

The Challenge: Mechanism for the Ketogenic Diet’s Impact on Epilepsy is Unknown
The ketogenic diet (KD), a low-carbohydrate and high-fat diet, has been shown for years to be an effective treatment for refractory epilepsy.1 The underlying mechanism of how this diet reduces neurological disease symptoms has been elusive for some time. The ketogenic diet is not utilized often as a treatment option due to difficulty with dietary compliance as well as a large number of possible side effects.2 Understanding the underlying mechanism better may allow for direct treatment that can circumvent having to use the ketogenic diet for treatment.
Previous studies in mice and humans identified changes in the gut microbiota as a result of switching to a ketogenic diet.3,4 Several other disease symptoms have been shown to be responsive to diet-induced alterations in the gut microbiota.5,6 Understanding what was already known about the ketogenic diet, epileptic neurological signaling, and the gut microbiome, researchers hypothesized that the ketogenic diet’s effect on the gut microbiome was leading to a shift in the gut’s secreted metabolome and, as a result, a direct change in neurological signaling.7
Metabolon Insight: Metabolites Produced by Gut Microbiota Impact Seizures
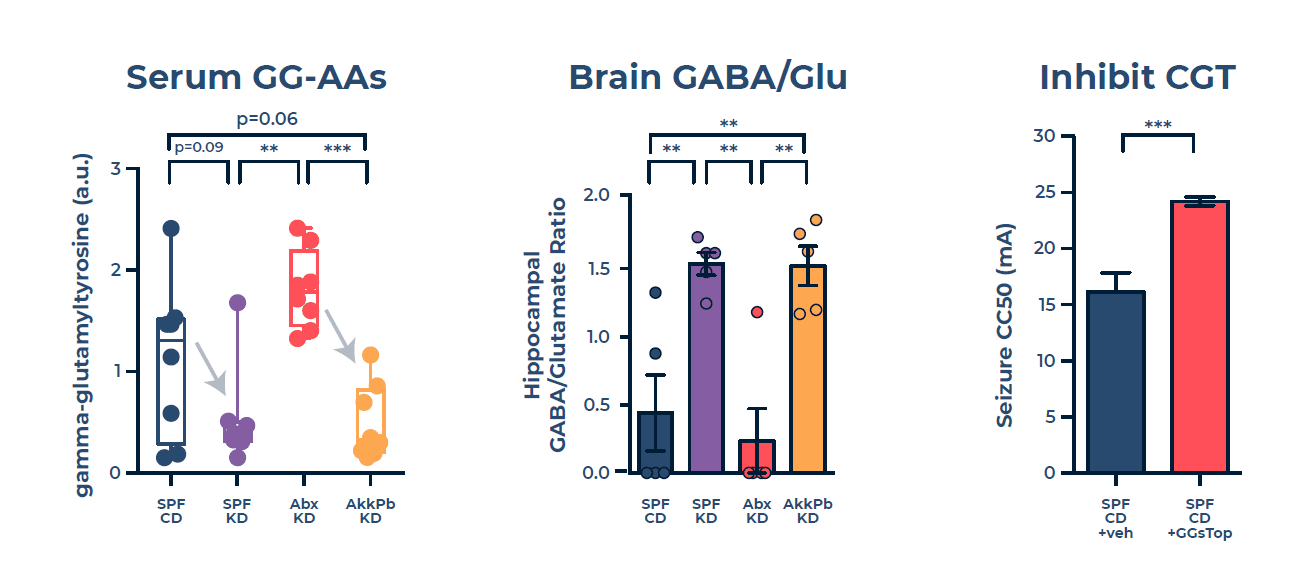
To test this hypothesis, the researchers set up experiments using a genetically engineered mouse model with temporal lobe epilepsy. They fed the mice with a control diet or ketogenic diet and treated them with either antibiotics (removing key gut microbiota) or probiotics (adding in key gut microbiota). Both the ketogenic diet and probiotic treated mice were found to be “seizure-protected” compared to the control diet and antibiotics treated group. Next, the Metabolon Global Discovery Panel compared levels of key metabolites. The service identified hundreds of metabolites, with a large portion of those with significantly altered levels belonging to a class of metabolites called gamma-glutamylated amino acids (GG-AAs). The GG-AAs were found to be reduced in the seizure-protected mice, illuminating that the GG-AAs level was significantly correlated to the number of seizures in mice.
A previous study by Cooper et al. showed that the levels of these GG-AAs can impact the level of key neurotransmitters in the brain such as gamma-aminobutyric acid (GABA).8 Thus, the researchers performed further metabolomics in the hippocampus, which is a major lobe in the brain that is a driver of seizure activity, to interrogate changes in GABA and glutamate levels. They identified that there were elevated levels of both GABA and glutamate in the seizure-protected groups, with an elevated increase in GABA compared to glutamate. The rationale was that in the KD and probiotic group, the reduction in GG-AAs produced by the gut microbiome directly led to a reduction in the balance of glutamate to GABA in the brain and therefore an increased GABA/glutamate ratio in the hippocampus. Both metabolomics studies identified changes in key metabolites that are produced by the gut microbiota and found in a central region of the brain in the seizure-protected mice, resulting from the ketogenic diet and probiotics.
The Solution: Utilize Inhibitor to Mimic Ketogenetic Diet Seizure Reduction
Having gained key mechanistic insight into how the ketogenic diet reduces seizures, the Hsiao lab aimed to target this mechanism to circumvent having to administer the ketogenic diet/probiotics. They utilized an inhibitor called GGsTOP, which inhibits the enzyme gamma-glutamyltranspeptidase (GGT) and blocks gamma-glutamination of amino acids. The administration of GGsTOP inhibited GGT and suggests this leads to restriction of the production of GG-AAs, which ultimately leads to a significant increase in seizure-protection of mice with epilepsy. This highlights a possible future treatment method for directly reducing seizures in patients with refractory epilepsy while avoiding the side effects and difficulties of the ketogenic diet.
The Outcome: Clinical Trials Started to Investigate GGT Inhibitor to Treat Epilepsy
By identifying key steps in the mechanism of a ketogenic diet resulting in seizure-reduction in refractory-epilepsy, the researchers made great progress in revealing usable biomarkers and potential treatments moving forward. Their results demonstrated that the lower level of GGT activity is correlated with seizure-protection, paving the way for this to potentially serve as a biomarker for epileptic patients who could benefit from a ketogenic diet, probiotics, or use of a GGT inhibitor to promote seizure-protection. This has laid a path forward to further examine this mechanism of diet-induced changes in the gut microbiota modulating neural activity in refractory-epilepsy. The researchers started human clinical trials to investigate GGT inhibitor and other gut microbiota further. Additionally, this study demonstrates the power of using metabolomics in studying gut-microbiota-induced changes in metabolite levels, as well as the altered levels of metabolites such as neurotransmitters in specific areas in the brain. Bringing the results of both metabolomic experiments together provides valuable insight into the mechanistic modulation the gut microbiota has on neurological activity and can be applied to studying other neurological diseases.
References
1. Kwan P, Brodie MJ. Early Identification of Refractory Epilepsy. New England Journal of Medicine. 2000;342(5):314-319. doi:10.1056/NEJM200002033420503
2. Freeman JM, Kossoff EH. Ketosis and the Ketogenic Diet, 2010: Advances in Treating Epilepsy and Other Disorders. Advances in Pediatrics. 2010;57(1):315-329. doi:10.1016/j.yapd.2010.08.003
3. Klein M, Newell C, Bomhof MR, et al. Metabolomic Modeling To Monitor Host Responsiveness to Gut Microbiota Manipulation in the BTBR(T+tf/j) Mouse. Journal of proteome research. Published online 2016. doi:10.1021/acs.jproteome.5b01025
4. Newell C, Bomhof MR, Reimer RA, Hittel DS, Rho JM, Shearer J. Ketogenic diet modifies the gut microbiota in a murine model of autism spectrum disorder. Molecular Autism. 2016;7(1):37. doi:10.1186/s13229-016-0099-3
5. Buffington SA, Di Prisco GV, Auchtung TA, Ajami NJ, Petrosino JF, Costa-Mattioli M. Microbial Reconstitution Reverses Maternal Diet-Induced Social and Synaptic Deficits in Offspring. Cell. 2016;165(7):1762-1775. doi:10.1016/j.cell.2016.06.001
6. Koeth RA, Wang Z, Levison BS, et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013;19(5):576-585. doi:10.1038/nm.3145
7. Olson CA, Vuong HE, Yano JM, Liang QY, Nusbaum DJ, Hsiao EY. The Gut Microbiota Mediates the Anti-Seizure Effects of the Ketogenic Diet [published correction appears in Cell. 2018 Jul 12;174(2):497]. Cell. 2018;173(7):1728-1741.e13. doi:10.1016/j.cell.2018.04.027
8. Cooper AJL, Jeitner TM. Central Role of Glutamate Metabolism in the Maintenance of Nitrogen Homeostasis in Normal and Hyperammonemic Brain. Biomolecules. 2016;6(2):E16. doi:10.3390/biom6020016




